Psoriasic Arthritis
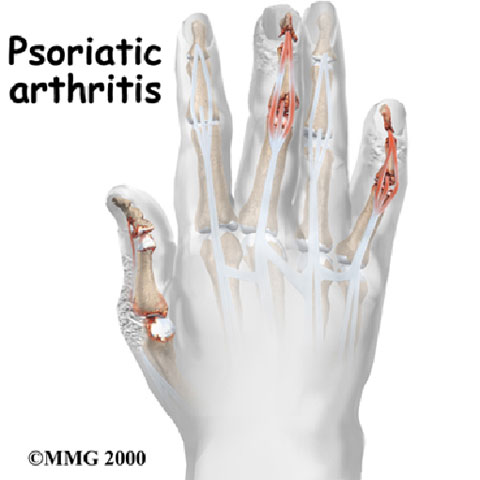 Psoriasic Arthritis (PsA) is a chronic inflammatory rheumatic disease characterised by an arthritis seronegative to the rheumatoid factor and associated with skin and/or nail psoriasis. In more simple terms, it is a condition of pain in the joints, associated with swelling and sense of warmth.
Psoriasic Arthritis (PsA) is a chronic inflammatory rheumatic disease characterised by an arthritis seronegative to the rheumatoid factor and associated with skin and/or nail psoriasis. In more simple terms, it is a condition of pain in the joints, associated with swelling and sense of warmth.
PsA belongs to the group of Seronegative Spondyloarthropathies, a group of rheumatic diseases that share the same genetic, pathogenic and clinical features. The group includes Ankylosing spondylitis (AS), Reactive Arthritis (ReA), arthritis associated with chronic bowel inflammatory diseases and undifferentiated seronegative spondyloarthropathies. The latter are also correlated with the histocompatibility antigen HLA-B27.
However, this definition does not clearly illustrate the nature of the disease and its many clinical symptoms. Indeed, PsA can be considered as a distinct clinical condition that can appear and disappear more often in patients with a family history of psoriasis, also if there are no psoriatic skin and/or nail lesions. Moreover, only a part of psoriasis patients (about 30%) develops an arthropathic form of psoriasis, and the onset, course and severity of the skin and rheumatologic outcomes – if both present together – are seldom correlated with each other. The only exceptions are a higher prevalence of PsA in the most severe cutaneous forms and a greater association between psoriatic onychopathy and the inflammatory involvement of the distal interphalangeal joints.
Therefore, it is believed that psoriasis and PsA may be independent consequences of a combination of common genetic and/or environmental factors, rather than the expression on the skin and joints of the same disorder of the immune system.



